
Orthodontic Brackets apply gentle, continuous pressure to facilitate bone remodeling. This gradually moves teeth into alignment. The process is the cornerstone of modern orthodontic treatment. It effectively transforms smiles. Treatment typically lasts 18 to 36 months. Dental Brackets, including Sapphire Brackets and Active Self Ligating Brackets, are essential components. An Orthodontic Products Manufacturer ensures their quality. Orthodontic Brackets and Arch Wires work together for precise tooth movement.
Key Takeaways
- Orthodontic brackets use gentle pressure to move teeth. This pressure helps bones change. This makes teeth straight over time.
- The archwire connects all brackets. It guides teeth into place. Different wires work for different stages of treatment.
- Good care is important with brackets. Brush often and avoid certain foods. Retainers keep teeth straight after treatment.
The Anatomy and Function of Orthodontic Brackets

Components of Orthodontic Brackets
Orthodontic treatment relies on small, precisely engineered components. The bracket itself forms the central piece of this system. It attaches directly to the tooth surface. Manufacturers create these essential Orthodontic Brackets from various materials. Stainless steel is a common choice. It offers a balance of cost, strength, and corrosion resistance. Specific alloys like 17-4 PH provide superior mechanical properties. Cobalt-chromium alloys present an alternative. They feature excellent biocompatibility and reduced nickel content. This makes them suitable for nickel-sensitive patients. Titanium and its alloys are also used. They offer superior biocompatibility, excellent corrosion resistance, and low allergic potential. Some brackets feature precious metal coatings. These coatings, often gold, platinum, or palladium, provide aesthetic value and inert surfaces.
Different designs of brackets cater to various patient needs and treatment goals. Metal braces use stainless steel bands, brackets, and wires. Ligatures hold the archwire in place. These are visible but allow for customizable ligature colors. Ceramic braces, also known as clear braces, function similarly. They use tooth-colored brackets, wires, and ligatures for a less noticeable appearance. However, they are more fragile. Lingual braces are placed on the back surfaces of the teeth. This makes them discreet. Self-ligating braces resemble traditional metal braces. They utilize a built-in system to secure the archwire instead of elastic ligatures. Examples include the DAMON ULTIMA™ SYSTEM and Damon™ Q2. Aesthetic options like Symetri™ Clear offer advanced ceramic technology.
The Role of the Archwire
The archwire connects all the brackets. It acts as the primary force-generating component. The archwire guides teeth into their correct positions. Its material composition significantly influences its effectiveness in tooth movement.
| Archwire Material | Surface Roughness (mean Ra µm) | Coefficient of Friction | Impact on Tooth Movement |
|---|---|---|---|
| Stainless Steel | 0.25 (smoothest) | 0.25 (lowest) | Reduced frictional forces, efficient for precise adjustments in later stages |
| Beta-Titanium | Intermediate | 0.28 | Relatively low friction, moderate control over tooth movement |
| NiTi | 0.35 (higher than SS and Beta-Ti) | 0.30 | Higher frictional resistance, but superelasticity provides consistent forces for effective movement |
| Esthetic Archwires | 0.40 (highest) | 0.35 (highest) | High friction, can slow down tooth movement process, potentially extending treatment duration |
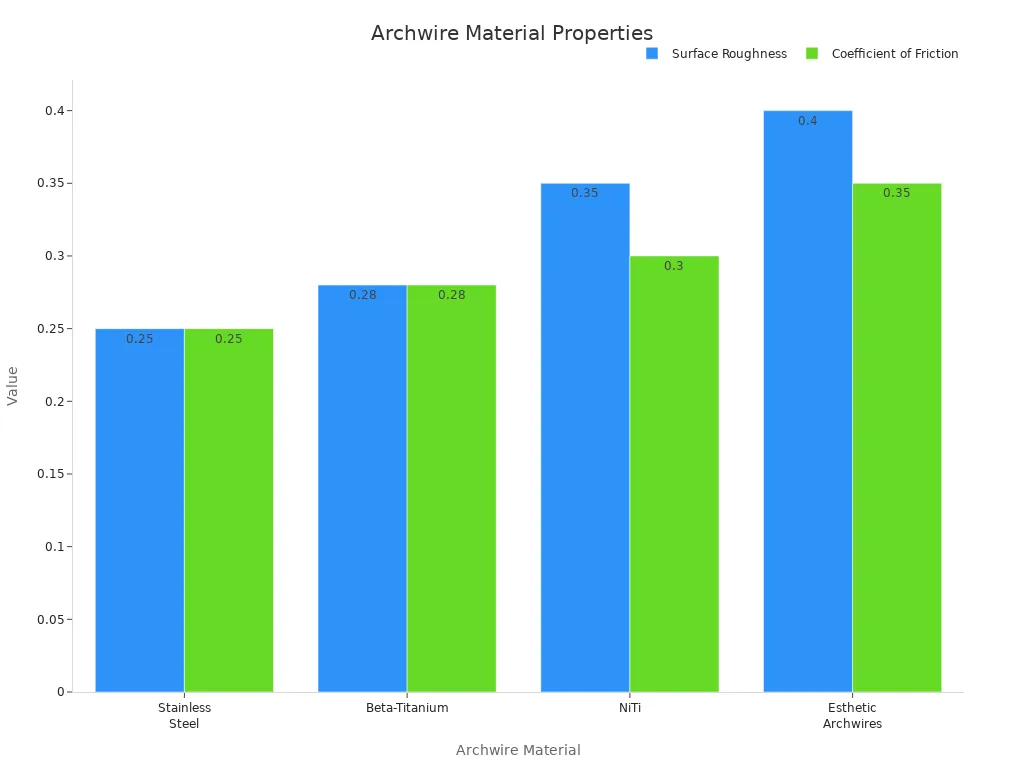
Stainless steel archwires are suitable for high-stress applications. They provide precise control due to their high mechanical strength and low frictional resistance. NiTi archwires are ideal for initial alignment and leveling stages. They offer consistent forces for large tooth movements. Their superelasticity and shape memory minimize patient discomfort. Esthetic archwires benefit patients prioritizing appearance. However, their lower mechanical strength and higher frictional resistance require judicious use. They work best for less demanding phases or as auxiliary wires.
Archwires come in various shapes and sizes.
- Shapes: Archwires are available in two primary cross-sectional shapes:
- Round: These wires are circular. They are typically used in the initial stages of treatment for leveling and aligning teeth due to their elasticity.
- Rectangular: These wires can be square or rectangular. They are generally introduced in later stages of treatment. They provide better control over tooth movement by fitting snugly into the rectangular wire slot of the bracket.
- Sizes: The ‘size’ of an archwire refers to its cross-section or thickness. A smaller cross-section results in a more elastic and less stiff wire, assuming the material is the same. The fit of the rectangular wire within the bracket slot can vary. It can range from a loose fit in earlier stages to a snug fit by the end of treatment. This indicates progression in wire size.
Ligatures, Ties, and Elastics
Ligatures and ties secure the archwire to the brackets. They ensure the archwire applies consistent pressure.
- Elastic Ties: These are small rubber bands. They hold the archwire in place. They come in various colors for customization. They help ensure proper tension and consistent pressure.
- Wire Ligature Ties: Crafted from stainless steel, these offer superior strength and durability. They secure the archwire tightly to the brackets for precise tooth movement and additional control.
Elastic ligatures can be loose or connected. Loose elastic ligatures offer flexibility in treatment. They provide precise control over the number used. Connected elastic ligatures are pre-connected. They allow for quicker application and easy, uniform placement around brackets. This reduces chair time.
Orthodontic elastics, also known as rubber bands, apply additional force. Braces alone cannot always achieve certain tooth movements. Elastics attach to tiny hooks on selected upper and lower brackets. The orthodontist custom-selects the configuration of elastics. They can connect teeth in the upper jaw to teeth in the lower jaw. They can also connect different teeth within the same jaw. This depends on the specific desired movement for individual or groups of teeth.
Elastics play a crucial role in applying pressure on teeth and the jaw. They move them into desired positions. They help address bite issues like overbites, underbites, and crossbites. They guide teeth into proper alignment. Elastics can also help level uneven or tilted teeth.
| Elastic Type | Function |
|---|---|
| Class I elastics | Close gaps between teeth, running from the upper first or second molar hook to the upper cuspid hook. |
| Class II elastics | Reduce an overjet by retracting upper teeth and moving lower teeth forward. |
| Class III elastics | Correct an underbite by retracting lower teeth and advancing upper teeth. |
| Vertical elastics | Link upper teeth with lower teeth to help with open bites. |
Elastics apply constant pressure to align both jaws. This improves bite function. They help shift the jaw’s position. This is crucial for patients with skeletal discrepancies. It leads to a more balanced facial appearance and improved function. When used correctly, elastics speed up the overall alignment process. They apply targeted pressure to specific areas. This encourages faster tooth movement and treatment progress.
The Science Behind Tooth Movement with Orthodontic Brackets
Bone Remodeling: Resorption and Apposition
Orthodontic tooth movement fundamentally relies on bone remodeling. This biological process involves the continuous breakdown and rebuilding of alveolar bone. When forces apply to a tooth, the periodontal ligament (PDL) experiences areas of compression and tension. On the compression side, bone resorption occurs. This process creates space for the tooth to move. Osteoclasts, specialized cells, activate through a sterile inflammatory response. Proinflammatory cytokines trigger this response. These cytokines induce the expression of RANKL (receptor activator of nuclear factor-κB ligand), a member of the tumor necrosis factor (TNF) family. RANKL then binds to its receptor, RANK, which initiates osteoclastogenesis, the formation of osteoclasts.
Osteoblast lineage cells, such as PDL cells and osteocytes, sense orthodontic forces. They produce several cytokines. RANKL is the most important cytokine promoting osteoclastogenesis. Osteoblasts primarily supply RANKL. Osteocytes embedded within the bone matrix, T lymphocytes in inflammatory conditions, and PDL cells also produce RANKL. Other inflammatory cytokines, including interleukin-1, tumor necrosis factor-α, and prostaglandin E2, also promote osteoclastogenesis during tooth movement.
The RANK/RANKL/OPG system plays a central role in controlling osteoclast activity:
- RANKL (Receptor Activator of Nuclear factor Kappa-Β Ligand): Osteoblasts and PDL cells express RANKL. It binds to RANK receptors on osteoclast precursors. This promotes their maturation into active osteoclasts.
- OPG (Osteoprotegerin): Osteoblasts produce OPG. It acts as a decoy receptor. OPG binds to RANKL, preventing its interaction with RANK. This inhibits osteoclastogenesis.
TNF-α-induced osteocyte necroptosis also enhances osteoclastogenesis and alveolar bone resorption on the compression side. This involves the release of inflammatory factors, including damage-associated molecular patterns (DAMPs). Conversely, on the tension side, bone apposition occurs. Osteoblasts deposit new bone, filling the space created by tooth movement. This coordinated process of resorption and apposition allows teeth to shift into their desired positions.
Applying Continuous Gentle Pressure
The application of continuous gentle pressure is paramount for effective orthodontic treatment. This consistent force initiates and sustains the biological processes necessary for tooth movement. Intermittent or inconsistent pressure can disrupt the remodeling cycle. This interruption often leads to prolonged treatment times or instability in the final orthodontic outcome. Therefore, consistent and continuous force application is crucial.
Orthodontic appliances, including the various types of Orthodontic Brackets, deliver these forces. The archwire, secured by ligatures or self-ligating mechanisms, transmits the force to the teeth. This gentle, continuous pressure stimulates the cells within the periodontal ligament and alveolar bone. It triggers the cascade of events leading to bone resorption on one side and bone apposition on the other. The precise control of force magnitude and direction ensures efficient and predictable tooth movement.
Biological Response to Orthodontic Brackets
Orthodontic forces elicit a complex biological response at the cellular and molecular levels. This response involves various mediators that orchestrate bone remodeling. Several biological markers indicate the tissue’s reaction to these forces. Aspartate aminotransferase (AST), a soluble enzyme, releases upon cell death. Its activity levels in gingival crevicular fluid (GCF) reflect periodontal tissue destruction. AST levels often peak in the first week of orthodontic force application. This suggests its potential as a marker for monitoring tooth movement. Lactate dehydrogenase (LDH) activity in GCF also serves as a diagnostic tool. Leptin, a polypeptide hormone, shows decreased concentration in GCF during tooth movement, indicating its role as a mediator.
General biological response components include neurotransmitters, arachidonic acid, growth factors, metabolites, cytokines, colony-stimulating factors, and enzymes like cathepsin K and matrix metalloproteinases (MMPs). These substances synthesize and release in response to orthodontic forces. They initiate the bone remodeling process. Interleukin-1 beta (IL-1β) shows a significant increase in GCF shortly after force application, for example, one day after ligature insertion. Soluble RANKL (sRANKL) also releases during an early phase response. Time-related increases in salivary levels have been reported.
However, excessive orthodontic forces can lead to adverse biological responses. These include unnecessary tissue damage in tooth-supporting structures and the dental pulp. Changes in dental pulp histomorphology can occur. These changes include circulatory disturbances, congested and dilated blood vessels, odontoblastic degeneration, vacuolization, edema of pulp tissues, fibrotic changes, disruption of the odontoblastic layer, and incomplete necrosis. Excessive forces also increase levels of neuropeptides such as Substance P (SP) and Calcitonin Gene-Related Peptide (CGRP). These neuropeptides can trigger vasodilation, edema, immune system activation, and recruitment of inflammatory cells. Elevated levels of C-Fos (a transcription factor) and MMP-9 (an enzyme degrading extracellular matrix) also indicate damage to pulp tissue. Severe orthodontic forces lead to significantly higher CGRP levels compared to moderate forces. Therefore, orthodontists carefully manage force levels to optimize tooth movement while minimizing potential harm.
Your Journey with Modern Orthodontic Brackets

Initial Consultation and Treatment Planning
The orthodontic journey begins with a thorough initial consultation. Orthodontists use several diagnostic tools to understand a patient’s oral health. These include X-rays, such as panoramic X-rays for a full mouth view, cephalometric projections for jaw and facial profile analysis, and Cone Beam CT for detailed 3D imaging. They also take facial and dental photographs, impressions or digital scans of teeth, and utilize digital imaging and intraoral cameras. A thorough clinical examination gathers essential data. This detailed assessment helps create an individualized treatment plan. This plan considers the patient’s mouth structure, dental history, and lifestyle factors. It addresses specific alignment issues like overcrowding or bite problems. For children, future growth and development are crucial. Adults often prefer discreet options. The plan also considers patient preferences for follow-up intervals, cleaning difficulty, and treatment duration.
Adjustments and Progress with Orthodontic Brackets
Regular adjustment appointments are vital for progress. The frequency of these visits varies by treatment type:
| Treatment Type | Typical Appointment Frequency |
|---|---|
| Traditional Braces | Every 4-6 weeks |
| Ceramic Braces | Every 4-6 weeks |
| Self-ligating Braces | Every 8 weeks |
| Invisalign | Every 6-10 weeks |
| Other Clear Aligners | Every 6-8 weeks |
During an adjustment, the orthodontist reviews progress and addresses concerns. They remove elastic ligatures and the archwire, if necessary. They examine brackets, wires, and bands, making minor repairs. They then place a new or existing archwire, adjusting its contour. Fresh elastics or ties secure the wire to each bracket. The orthodontist reviews instructions for interarch elastics and checks the bite for comfort. They use tools like orthodontic pliers, power chains, and measuring gauges.
Living with Orthodontic Brackets: Care and Expectations
Maintaining excellent oral hygiene is crucial with Orthodontic Brackets. Patients should brush their teeth multiple times daily, especially after meals, using toothpaste. An interproximal brush cleans hard-to-reach spaces. Flossing at least once a day prevents cavities. Rinsing with water after sugary drinks helps. Orthodontic toothbrushes and oral irrigators assist in cleaning around braces. Mobile apps can track cleaning routines. Patients should rinse with warm water or antimicrobial mouthwash in the morning. They should conduct a comprehensive cleaning routine in the evening.
Dietary restrictions are also important. Patients should avoid hard foods like nuts and hard candies, sticky foods such as taffy and caramel, and crunchy items like popcorn. Sugary and acidic foods increase cavity risk. Cutting food into small pieces and chewing slowly helps prevent damage to appliances.
The Importance of Retainers After Orthodontic Brackets
After active treatment, retainers prevent teeth from shifting back. Various types exist:
- Hawley Retainers: These feature an acrylic base and a metal wire.
- Clear Plastic Retainers (Essix Retainers): These are nearly invisible and fit snugly.
- Fixed (Permanent) Retainers: Thin metal wires bond to the back of front teeth.
- Vacuum Form Retainers (VFR): Aesthetic and comfortable, but can wear down.
- Fixed Lingual Retainers: Wires bonded to the back of teeth, offering continuous retention.
The recommended duration for retainer wear varies. Initially, patients wear retainers 24 hours a day for several months, typically 4 to 10 months. After this, they transition to nightly wear. Many orthodontists recommend continued nightly use for a lifetime to prevent relapse.
Modern orthodontic treatments effectively align teeth. They use precise forces and biological bone remodeling. This process enhances patient cooperation and treatment success. Patients achieve a healthy, aligned smile and improved oral health. This outcome prevents dental problems and improves overall well-being.
| Treatment Type | Success Rate | Additional Factors |
|---|---|---|
| Traditional Braces | 88-90% | Treatment planning, retention |
| Invisalign (malocclusion correction) | 88-90% | N/A |
| Clear Aligners (mild to moderate cases) | 80-96% | Patient compliance, case complexity, patient age, adherence to protocols |
- Prevents Tooth Decay and Gum Disease: Straight teeth are easier to clean, reducing plaque buildup and the risk of cavities, gingivitis, and periodontitis.
- Improves Bite Function and Jaw Alignment: Corrects malocclusions (e.g., overbites, underbites) to enhance chewing efficiency and relieve jaw strain, preventing TMJ-related symptoms.
- Minimizes Uneven Tooth Wear: Ensures even distribution of bite force, protecting enamel from wear, sensitivity, chips, and fractures.
- Protects Against Tooth Damage and Loss: Reduces vulnerability of misaligned teeth to accidental damage and strengthens their structure, decreasing the need for future restorative procedures.
- Supports Jawbone Health: Proper tooth positioning stimulates the jawbone during chewing, maintaining bone density and preserving facial structure.
- Enhances Daily Oral Hygiene: Makes thorough cleaning easier, reducing plaque accumulation and the risk of cavities, gum disease, and bad breath, leading to long-term oral health.
FAQ
How do orthodontic brackets move teeth?
Brackets apply gentle, continuous pressure. This pressure stimulates bone remodeling. Bone breaks down on one side and rebuilds on the other. This process gradually shifts teeth into alignment.
Why are retainers necessary after braces?
Retainers prevent teeth from shifting back to their original positions. They stabilize the teeth in their new alignment. This ensures the long-term success of orthodontic treatment.
How should patients care for their teeth with brackets?
Patients must brush multiple times daily and floss regularly. They should use specialized tools for cleaning around brackets. Avoiding hard, sticky, and sugary foods also protects the appliances.
Post time: Jan-20-2026


